| << Chapter < Page | Chapter >> Page > |
General laboratory testing for hepatitis begins with blood testing to examine liver function ( [link] ). When the liver is not functioning normally, the blood will contain elevated levels of alkaline phosphatase , alanine aminotransferase (ALT), aspartate aminotransferase (AST), direct bilirubin , total bilirubin, serum albumin, serum total protein, and calculated globulin, albumin/globulin (A/G) ratio. Some of these are included in a complete metabolic panel (CMP), which may first suggest a possible liver problem and indicate the need for more comprehensive testing. A hepatitis virus serological test panel can be used to detect antibodies for hepatitis viruses A, B, C, and sometimes D. Additionally, other immunological and genomic tests are available.
Specific treatments other than supportive therapy, rest, and fluids are often not available for hepatitis virus infection, except for HCV, which is often self-limited. Immunoglobulins can be used prophylactically following possible exposure. Medications are also used, including interferon alpha 2b and antivirals (e.g., lamivudine , entecavir , adefovir , and telbivudine ) for chronic infections. Hepatitis C can be treated with interferon (as monotherapy or combined with other treatments), protease inhibitors, and other antivirals (e.g., the polymerase inhibitor sofosbuvir ). Combination treatments are commonly used. Antiviral and immunosuppressive medications may be used for chronic cases of HEV. In severe cases, liver transplants may be necessary. Additionally, vaccines are available to prevent infection with HAV and HBV. The HAV vaccine is also protective against HEV. The HBV vaccine is also protective against HDV. There is no vaccine against HCV.
Learn more information about heptatitisvirus infections.
Hepatitis B was once a leading on-the-job hazard for health-care workers. Many health-care workers over the years have become infected, some developing cirrhosis and liver cancer. In 1982, the CDC recommended that health-care workers be vaccinated against HBV, and rates of infection have declined since then. Even though vaccination is now common, it is not always effective and not all individuals are vaccinated. Therefore, there is still a small risk for infection, especially for health-care workers working with individuals who have chronic infections, such as drug addicts, and for those with higher risk of needle sticks, such as phlebotomists. Dentists are also at risk.
Health-care workers need to take appropriate precautions to prevent infection by HBV and other illnesses. Blood is the greatest risk, but other body fluids can also transmit infection. Damaged skin, as occurs with eczema or psoriasis, can also allow transmission. Avoiding contact with body fluids, especially blood, by wearing gloves and face protection and using disposable syringes and needles reduce the risk of infection. Washing exposed skin with soap and water is recommended. Antiseptics may also be used, but may not help. Post-exposure treatment, including treatment with hepatitis B immunoglobulin (HBIG) and vaccination, may be used in the event of exposure to the virus from an infected patient. Detailed protocols are available for managing these situations. The virus can remain infective for up to seven days when on surfaces, even if no blood or other fluids are visible, so it is important to consider the best choices for disinfecting and sterilizing equipment that could potentially transmit the virus. The CDC recommends a solution of 10% bleach to disinfect surfaces. Centers for Disease Control and Prevention. “Hepatitis B FAQs for Health Professionals.” Updated August 4, 2016. http://www.cdc.gov/hepatitis/HBV/HBVfaq.htm. Finally, testing blood products is important to reduce the risk of transmission during transfusions and similar procedures.
Hepatitis involves inflammation of the liver that typically manifests with signs and symptoms such as jaundice, nausea, vomiting, joint pain, gray stool, and loss of appetite. However, the severity and duration of the disease can vary greatly depending on the causative agent. Some infections may be completely asymptomatic, whereas others may be life threatening. The five different viruses capable of causing hepatitis are compared in [link] . For the sake of comparison, this table presents only the unique aspects of each form of viral hepatitis, not the commonalities.
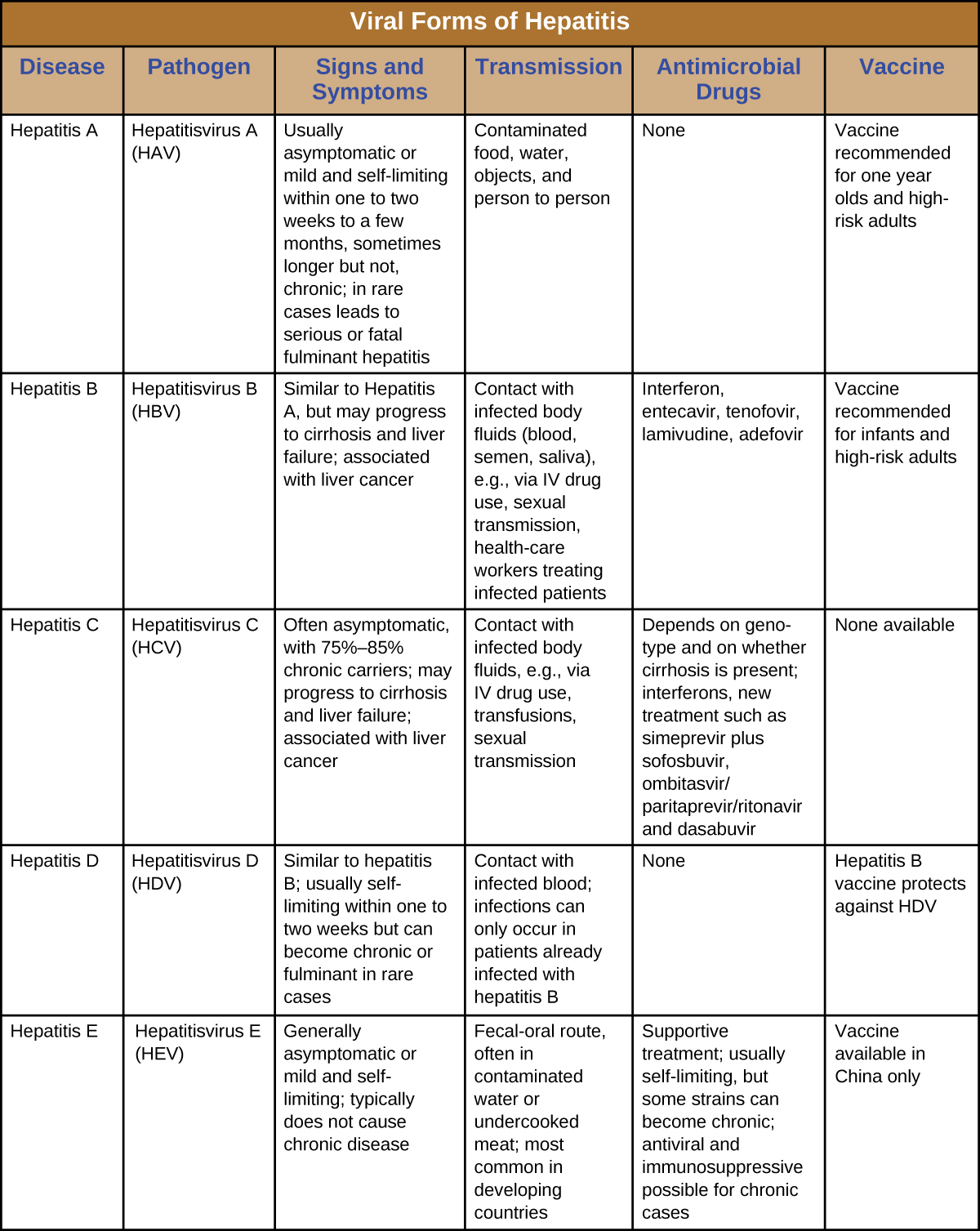
Which forms of viral hepatitis are transmitted through the fecal-oral route?

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?