| << Chapter < Page | Chapter >> Page > |
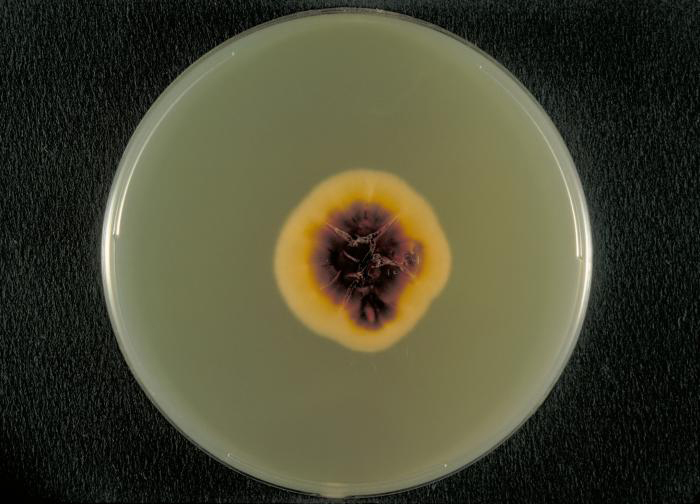
Several approaches may be used to diagnose tineas. A Wood’s lamp (also called a black lamp) with a wavelength of 365 nm is often used. When directed on a tinea, the ultraviolet light emitted from the Wood’s lamp causes the fungal elements (spores and hyphae) to fluoresce. Direct microscopic evaluation of specimens from skin scrapings, hair, or nails can also be used to detect fungi. Generally, these specimens are prepared in a wet mount using a potassium hydroxide solution (10%–20% aqueous KOH), which dissolves the keratin in hair, nails, and skin cells to allow for visualization of the hyphae and fungal spores. The specimens may be grown on Sabouraud dextrose CC (chloramphenicol/cyclohexamide), a selective agar that supports dermatophyte growth while inhibiting the growth of bacteria and saprophytic fungi ( [link] ). Macroscopic colony morphology is often used to initially identify the genus of the dermatophyte; identification can be further confirmed by visualizing the microscopic morphology using either a slide culture or a sticky tape prep stained with lactophenol cotton blue.
Various antifungal treatments can be effective against tineas. Allylamine ointments that include terbinafine are commonly used; miconazole and clotrimazole are also available for topical treatment, and griseofulvin is used orally.
Another cause of cutaneous mycoses is Aspergillus , a genus consisting of molds of many different species, some of which cause a condition called aspergillosis . Primary cutaneous aspergillosis, in which the infection begins in the skin, is rare but does occur. More common is secondary cutaneous aspergillosis, in which the infection begins in the respiratory system and disseminates systemically. Both primary and secondary cutaneous aspergillosis result in distinctive eschars that form at the site or sites of infection ( [link] ). Pulmonary aspergillosis will be discussed more thoroughly in Respiratory Mycoses ).

Primary cutaneous aspergillosis usually occurs at the site of an injury and is most often caused by Aspergillus fumigatus or Aspergillus flavus . It is usually reported in patients who have had an injury while working in an agricultural or outdoor environment. However, opportunistic infections can also occur in health-care settings, often at the site of intravenous catheters, venipuncture wounds, or in association with burns, surgical wounds, or occlusive dressing. After candidiasis, aspergillosis is the second most common hospital-acquired fungal infection and often occurs in immunocompromised patients, who are more vulnerable to opportunistic infections.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?