| << Chapter < Page | Chapter >> Page > |
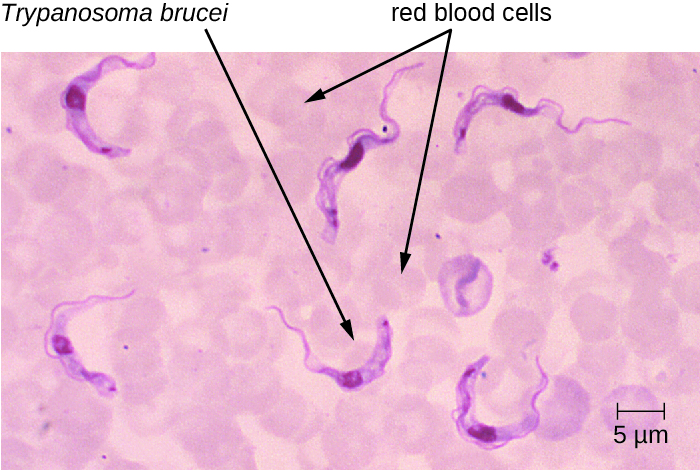
T. brucei is primarily transmitted to humans by the bite of the tsetse fly ( Glossina spp.). Soon after the bite of a tsetse fly, a chancre forms at the site of infection. The flagellates then spread, moving into the circulatory system ( [link] ). These systemic infections result in an undulating fever , during which symptoms persist for two or three days with remissions of about a week between bouts. As the disease enters its final phase, the pathogens move from the lymphatics into the CNS. Neurological symptoms include daytime sleepiness, insomnia, and mental deterioration. In EAT, the disease runs its course over a span of weeks to months. In contrast, WAT often occurs over a span of months to years.
Although a strong immune response is mounted against the trypanosome, it is not sufficient to eliminate the pathogen. Through antigenic variation , Trypanosoma can change their surface proteins into over 100 serological types. This variation leads to the undulating form of the initial disease. The initial septicemia caused by the infection leads to high fevers. As the immune system responds to the infection, the number of organisms decrease, and the clinical symptoms abate. However, a subpopulation of the pathogen then alters its surface coat antigens by antigenic variation and evades the immune response. These flagellates rapidly proliferate and cause another bout of disease. If untreated, these infections are usually fatal.
Clinical symptoms can be used to recognize the early signs of African trypanosomiasis. These include the formation of a chancre at the site of infection and Winterbottom’s sign . Winterbottom’s sign refers to the enlargement of lymph nodes on the back of the neck—often indicative of cerebral infections. Trypanosoma can be directly observed in stained samples including blood, lymph, CSF, and skin biopsies of chancres from patients. Antibodies against the parasite are found in most patients with acute or chronic disease. Serologic testing is generally not used for diagnosis, however, since the microscopic detection of the parasite is sufficient. Early diagnosis is important for treatment. Before the nervous system is involved, drugs like pentamidine (an inhibitor of nuclear metabolism) and suramin (mechanism unclear) can be used. These drugs have fewer side effects than the drugs needed to treat the second stage of the disease. Once the sleeping sickness phase has begun, harsher drugs including melarsoprol (an arsenic derivative) and eflornithine can be effective. Following successful treatment, patients still need to have follow-up examinations of their CSF for two years to detect possible relapses of the disease. The most effective means of preventing these diseases is to control the insect vector populations.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?