| << Chapter < Page | Chapter >> Page > |
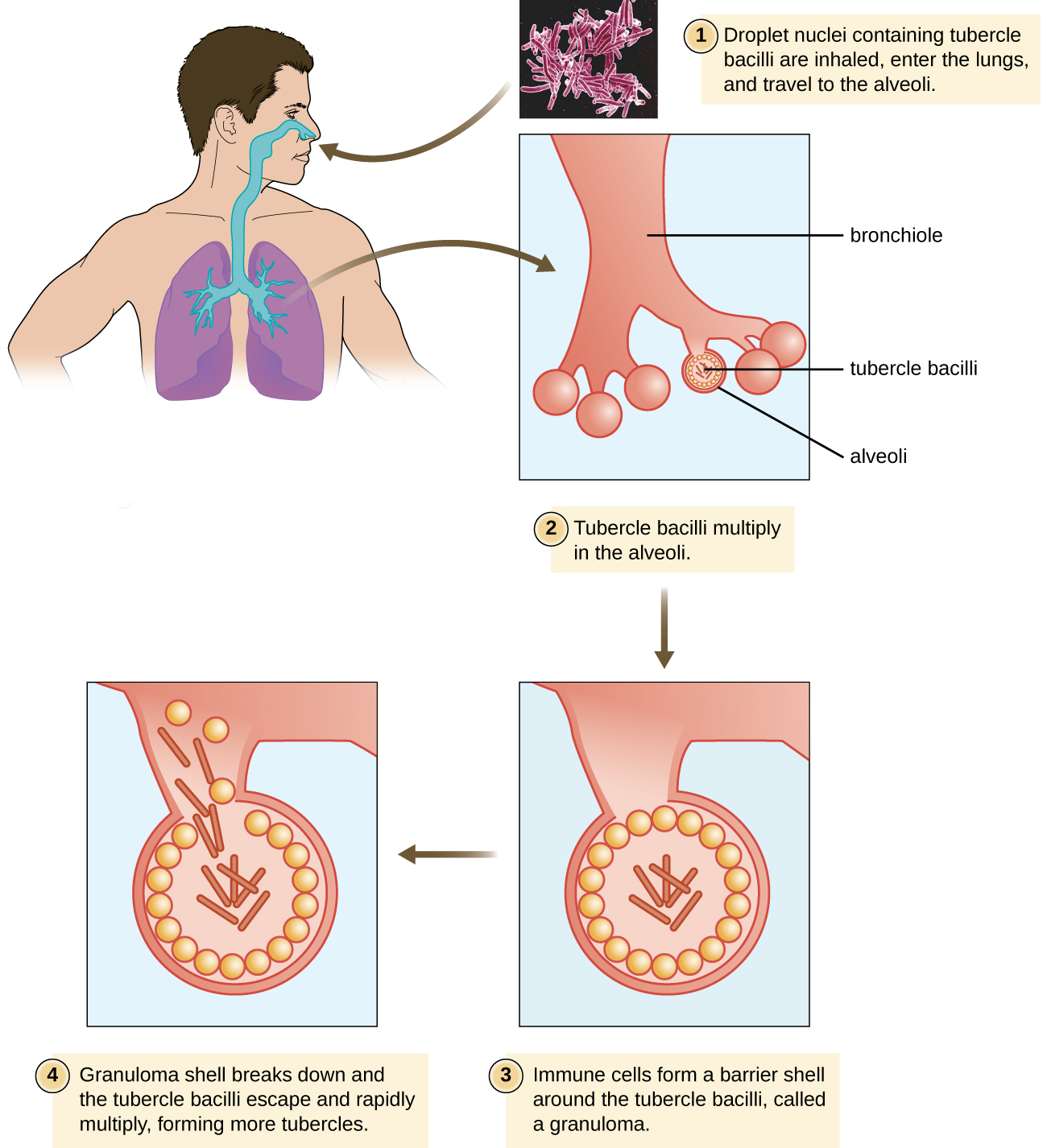
After inhalation, the bacteria enter the alveoli ( [link] ). The cells are phagocytized by macrophages but can survive and multiply within these phagocytes because of the protection by the waxy mycolic acid in their cell walls. If not eliminated by macrophages, the infection can progress, causing an inflammatory response and an accumulation of neutrophils and macrophages in the area. Several weeks or months may pass before an immunological response is mounted by T cells and B cells. Eventually, the lesions in the alveoli become walled off, forming small round lesions called tubercles . Bacteria continue to be released into the center of the tubercles and the chronic immune response results in tissue damage and induction of apoptosis (programmed host-cell death) in a process called liquefaction. This creates a caseous center, or air pocket, where the aerobic M. tuberculosis can grow and multiply. Tubercles may eventually rupture and bacterial cells can invade pulmonary capillaries; from there, bacteria can spread through the bloodstream to other organs, a condition known as miliary tuberculosis . The rupture of tubercles also facilitates transmission of the bacteria to other individuals via droplet aerosols that exit the body in coughs. Because these droplets can be very small and stay aloft for a long time, special precautions are necessary when caring for patients with TB, such as the use of face masks and negative-pressure ventilation and filtering systems.
Eventually, most lesions heal to form calcified Ghon complexes . These structures are visible on chest radiographs and are a useful diagnostic feature. But even after the disease has apparently ended, viable bacteria remain sequestered in these locations. Release of these organisms at a later time can produce reactivation tuberculosis (or secondary TB). This is mainly observed in people with alcoholism, the elderly, or in otherwise immunocompromised individuals ( [link] ).
Because TB is a chronic disease, chemotherapeutic treatments often continue for months or years. Multidrug resistant (MDR-TB) and extensively drug-resistant (XDR-TB) strains of M. tuberculosis are a growing clinical concern. These strains can arise due to misuse or mismanagement of antibiotic therapies. Therefore, it is imperative that proper multidrug protocols are used to treat these infections. Common antibiotics included in these mixtures are isoniazid, rifampin, ethambutol, and pyrazinamide.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?