| << Chapter < Page | Chapter >> Page > |
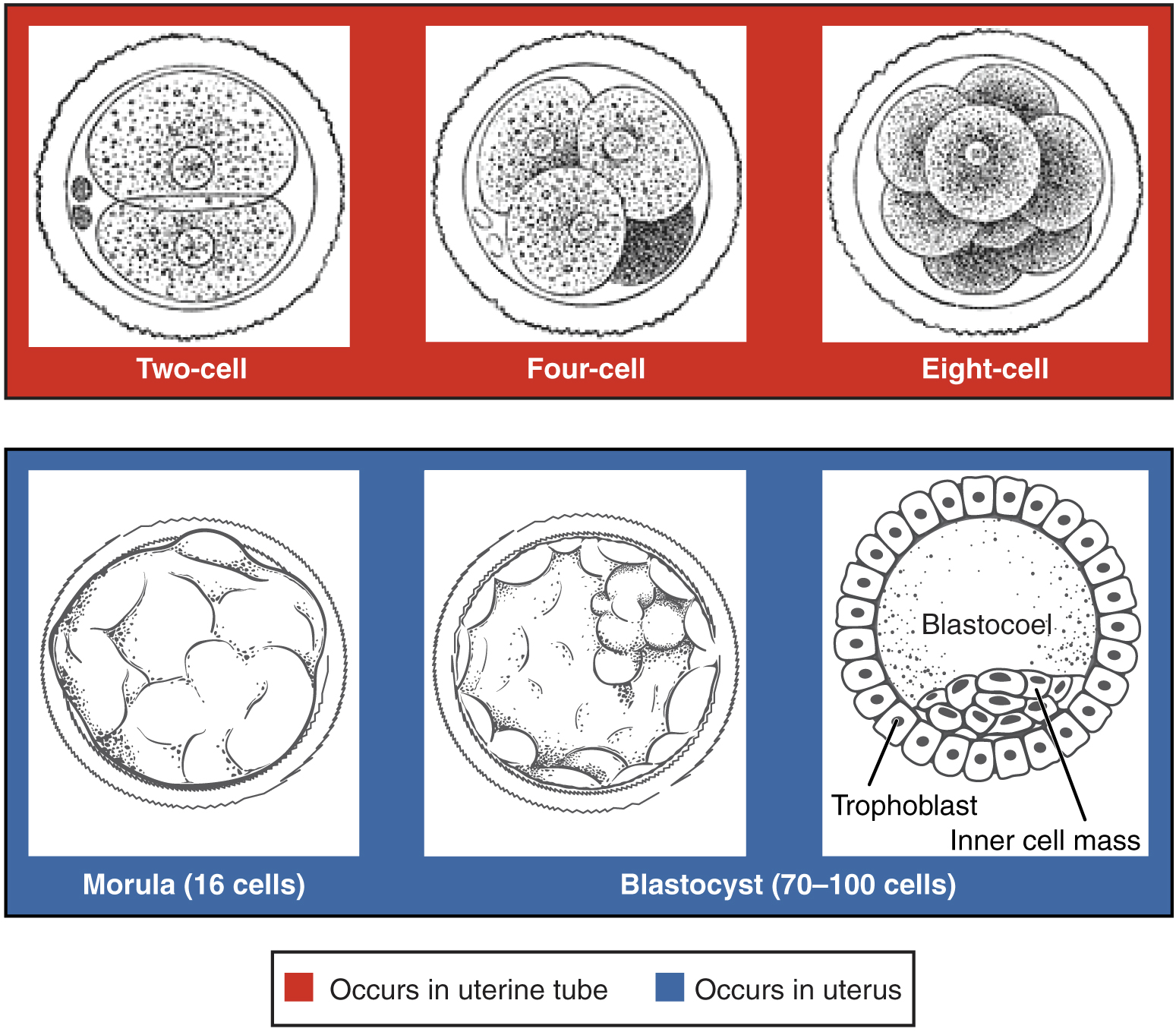
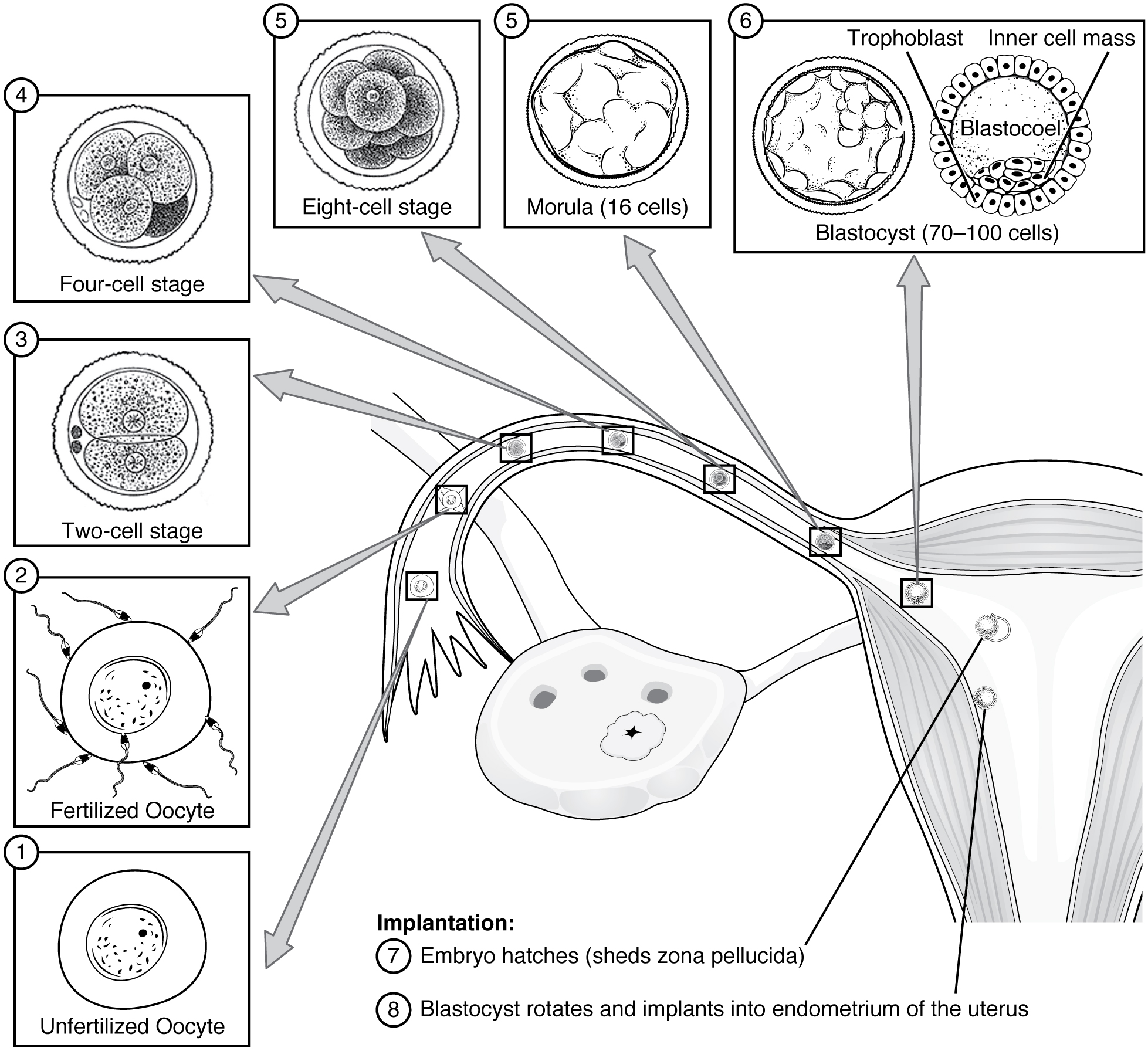
As the blastocyst forms, the trophoblast excretes enzymes that begin to degrade the zona pellucida. In a process called “hatching,” the conceptus breaks free of the zona pellucida in preparation for implantation.
View this time-lapse movie of a conceptus starting at day 3. What is the first structure you see? At what point in the movie does the blastocoel first appear? What event occurs at the end of the movie?
At the end of the first week, the blastocyst comes in contact with the uterine wall and adheres to it, embedding itself in the uterine lining via the trophoblast cells. Thus begins the process of implantation , which signals the end of the pre-embryonic stage of development ( [link] ). Implantation can be accompanied by minor bleeding. The blastocyst typically implants in the fundus of the uterus or on the posterior wall. However, if the endometrium is not fully developed and ready to receive the blastocyst, the blastocyst will detach and find a better spot. A significant percentage (50–75 percent) of blastocysts fail to implant; when this occurs, the blastocyst is shed with the endometrium during menses. The high rate of implantation failure is one reason why pregnancy typically requires several ovulation cycles to achieve.
When implantation succeeds and the blastocyst adheres to the endometrium, the superficial cells of the trophoblast fuse with each other, forming the syncytiotrophoblast , a multinucleated body that digests endometrial cells to firmly secure the blastocyst to the uterine wall. In response, the uterine mucosa rebuilds itself and envelops the blastocyst ( [link] ). The trophoblast secretes human chorionic gonadotropin (hCG) , a hormone that directs the corpus luteum to survive, enlarge, and continue producing progesterone and estrogen to suppress menses. These functions of hCG are necessary for creating an environment suitable for the developing embryo. As a result of this increased production, hCG accumulates in the maternal bloodstream and is excreted in the urine. Implantation is complete by the middle of the second week. Just a few days after implantation, the trophoblast has secreted enough hCG for an at-home urine pregnancy test to give a positive result.
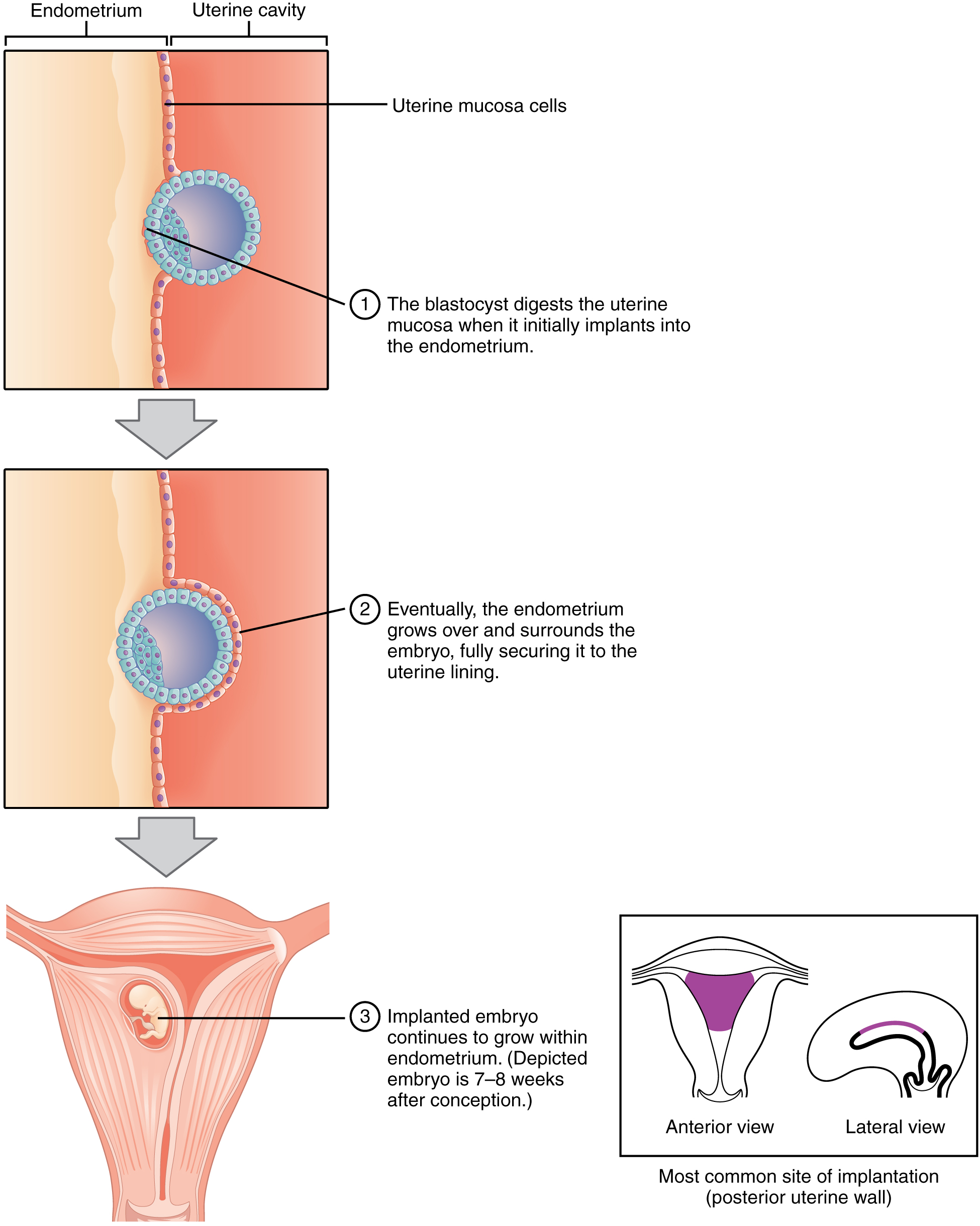
Most of the time an embryo implants within the body of the uterus in a location that can support growth and development. However, in one to two percent of cases, the embryo implants either outside the uterus (an ectopic pregnancy ) or in a region of uterus that can create complications for the pregnancy. If the embryo implants in the inferior portion of the uterus, the placenta can potentially grow over the opening of the cervix, a condition call placenta previa .

Notification Switch
Would you like to follow the 'Anatomy & Physiology' conversation and receive update notifications?